Summary 概括
Although Japan's healthcare delivery system is highly regarded internationally, the COVID-19 pandemic has exposed its structural problems. Behind these issues lies a history of medical care provisions supported mainly by an unrestricted, "free labeling" system, and independently financed private hospitals. In addition, patients have a high degree of freedom of choice under the Japanese medical insurance system, making it difficult to provide comprehensive and continuous health management from initial diagnosis and treatment (primary care), specialized treatment, to supporting a return to home, providing nursing care and lifestyle support. As Japan becomes a "super-aged" society with individuals over 65 making up over 30% of the population, the nature of medical care will have to undergo major changes. Medical care's basic function must still be the treatment and cure of patients, but the system will also have to provide support. That means conceiving of care in a way that treats a person's life with dignity and does not sacrifice life for treatment. The implementation of a family doctor function and the clarification of the functions and roles of small and medium-sized community-based hospitals that support this function, as well as the establishment of a community comprehensive care network with multidisciplinary cooperation that goes beyond medical care, should also be set forth in future regional medical care plans.
尽管日本的医疗服务体系在国际上享有盛誉,但新冠疫情暴露了其结构性问题。这些问题的背后,是日本医疗服务体系长期以来主要依靠不受限制的“自由标签”制度和自筹资金的私立医院支撑。此外,在日本医疗保险制度下,患者拥有高度的选择自由,这使得从最初的诊断和治疗(初级保健)、专科治疗,到支持患者回家、提供护理和生活支持,难以提供全面且持续的健康管理。随着日本迈入“超高龄社会”,65岁以上人口占总人口的30%以上,医疗保健的本质将不得不发生重大变化。医疗保健的基本功能仍然是治疗和治愈患者,但该系统也必须提供支持。这意味着,医疗保健的理念必须尊重患者的生命,而不是为了治疗而牺牲生命。落实家庭医生职能,明确支持该职能的中小型社区医院的功能和作用,建立超越医疗范畴的多学科合作的社区综合护理网络,也应在未来的区域医疗保健规划中得到明确。
Keywords: healthcare delivery system, medical insurance system, population ageing, medical care, Japan
关键词: 医疗服务体系、医疗保险制度、人口老龄化、医疗保健、日本
Introduction 介绍
Hospitals are believed to have originated in the Middle Ages as accommodations for pilgrims. These early hospitals were mainly institutions for the nursing of the poor, sick, and stranded. The Hospice de Beaune in Beaune, France, is the world's oldest sanatorium, established in the mid-15th century.
医院被认为起源于中世纪,最初是朝圣者的住所。这些早期的医院主要为贫困、患病和滞留者提供护理。法国博讷的博讷临终关怀院是世界上最古老的疗养院,建于15世纪中叶。
Later, the Elizabethan Poor Law of the 16th century in England created "Contagious Hospitals" as places to care for patients in isolation. The same laws created poorhouses but these were mainly institutions where workers were treated and then sent to work again. In the 19th century, as modern medicine developed, military medicine and military hospitals developed as separate systems.
后来,英国16世纪的伊丽莎白济贫法设立了“传染病医院”,作为隔离收治病人的场所。同样的法律也设立了济贫院,但这些机构主要为工人提供治疗,然后送他们回去工作。19世纪,随着现代医学的发展,军事医学和军事医院发展成为独立的系统。
Either way, all modern hospitals in Europe for the treatment of the general public developed either as religious hospitals or public hospitals for the poor. In contrast, "clinics" have completely different origins and developed separately.
无论如何,欧洲所有为大众服务的现代医院,要么发展成为宗教医院,要么发展成为面向穷人的公立医院。相比之下,“诊所”的起源则截然不同,各自发展。
In Japan, hospitals developed in an altogether different way. As a 2013 government report (1) states:
在日本,医院的发展方式截然不同。正如 2013 年的一份政府报告 ( 1 ) 所述:
"The difficulty of Japan's healthcare policy stems from the fact that, unlike in Western and Northern Europe, where national and municipal hospitals and other facilities are publicly owned, physicians have established medical corporations and private capital has been used to manage hospitals and other facilities (private ownership)".
日本医疗政策的困难在于,与西欧和北欧的国家和市立医院等设施为公有制不同,日本的医疗政策是由医生成立医疗法人,并由民间资本来管理医院等设施(私有制)” 。
"In the case of a publicly-owned system, governments can mandate reforms, such as how reforms have taken place in response to healthcare needs in some European countries recently".
“在公有制体系下,政府可以强制进行改革,就像最近一些欧洲国家为满足医疗保健需求而进行的改革一样” 。
"No other developed country as Japan has such a deregulated and market-dependent healthcare delivery system. In the case of Japan, publicly-owned healthcare facilities account for only 14% of all healthcare facilities and 22% of all hospital beds. Therefore, it has been difficult for Japan to do what other countries where healthcare institutions are publicly-owned can do systematically".
“没有哪个发达国家像日本一样,拥有如此放松管制、市场化运作的医疗服务体系。就日本而言,公立医疗机构仅占所有医疗机构的 14%,占所有病床的 22%。因此,日本很难做到其他医疗机构公立的国家能够系统地做到的事情。”
Characteristics of Japanese healthcare delivery system: Ownership-based medical care structure
日本医疗服务体系的特点:所有制型医疗结构
Professor Shuhei Ikai of Hitotsubashi University, in his book "A Theory of the Hospital Century" (2), states that the Japanese healthcare delivery system is characterized by an "ownership-based medical care structure", which he defines as having the following characteristics:
一桥大学的井井周平教授在其著作《医院世纪理论》( 2 ) 中指出,日本的医疗保健体系以“所有权型医疗保健结构”为特征,他将其定义为具有以下特征:
i) Free access with a high degree of freedom. This leads to bloated outpatient care. It means "if you wait for three hours, you can see a doctor on the same day. There are very few countries where this type of outpatient consultation is possible.
i ) 免费就诊,自由度高。 这导致门诊服务臃肿不堪。这意味着“只要等三个小时,就能当天就诊”。很少有国家能够提供这种门诊服务。
ii) Ownership of hospital beds by physicians in a system where any licensed physician has the freedom to choose where he or she opens their business and their specialty (free labeling). The functions of large hospitals and clinics are undifferentiated, and large hospitals also have outpatient departments, creating a competitive relationship between them. General practitioners have certain specialties, and both hospitals and clinics provide both primary and secondary care, which means offerings overlap.
ii ) 在任何执业医师都可以自由选择其执业地点和专科(自由标签)的体系下,医院床位归医生所有。 大型医院和诊所的功能没有区别,大型医院也设有门诊部,这使得它们之间存在竞争关系。全科医生拥有特定的专科,医院和诊所都提供初级和二级医疗服务,这意味着服务内容重叠。
iii) Direct employment of physicians by hospitals. It is the physicians attached to (i.e., employed by) the hospital who provide medical care using the hospital's medical resources. So-called open-type hospitals do not function in Japan.
iii ) 医院直接聘用医生。 指医院的附属医生( 即受聘于医院的医生)利用医院的医疗资源提供医疗服务。日本不存在所谓的开放式医院。
iv) High ratio of private hospitals and hospital bed stock. The historical development of Japanese hospitals is unique in that private clinics became hospitals with their own beds, and then became incorporated as medical corporations.
iv ) 私立医院比例高,病床存量大。 日本医院的历史发展比较独特,由私人诊所发展成为拥有独立病床的医院,再由私人诊所法人化成为医疗公司。
v) Decentralized distribution of hospital beds and expensive medical equipment. As a consequence of iii) and iv), each medical institution manages its own hospitals based on its own risk and judgment in a competitive relationship. As a result, the distribution of beds among facilities is decentralized, and each institution decides how it will invest capital. making it difficult to systematically allocate beds and equipment.
v ) 病床和昂贵医疗设备的分散分布。 由于 iii )和 iv )的缘故,各医疗机构在竞争关系中根据自身风险和判断来管理各自的医院。结果,各医疗机构的病床分配分散,由各机构自行决定如何投资,这使得系统地分配病床和设备变得困难。
vi) High specialization of general practitioners. Most general practitioners start their career through the medical office and resident physician system, then open their own practice, and many also have a specialty. This situation is quite different from that of general practitioners in other countries; in reality, Japanese general practitioners are able to provide not only primary care but also a certain level of secondary care.
六 ) 全科医生的专业化程度高。 大多数全科医生的职业生涯始于诊所和住院医师制度,之后开设自己的诊所,许多全科医生还拥有自己的专科。这种情况与其他国家的全科医生截然不同;实际上,日本的全科医生不仅能够提供初级护理,还能提供一定程度的二级护理。
vii) The lack of a family doctor (GP) system.
vii ) 缺乏家庭医生(GP)制度。
viii) Medical office system and egalitarian hiring. Because both resident physicians and doctors in private practice both have the same level of specialization, a system of specialized doctors does not work.
8 ) 医疗办公室制度和平等雇佣。由于住院医师和私人执业医生的专业化程度相同,专科医生制度无法发挥作用。
Japan's modern medical care system has taken shape since the Meiji era. This extremely stable and immutable system has come to be a defining factor for medical policy, and, as a result, medical policy has only progressed gradually.
日本的现代医疗制度自明治时代起就已形成,这种极其稳定、不可改变的制度成为医疗政策的决定性因素,医疗政策也因此得以循序渐进地发展。
An evaluation of Japan's healthcare system to date
对日本医疗体系现状的评估
Japan's healthcare system is highly regarded internationally, as the country achieved universal healthcare coverage in the 1960s. There are very few treatments that are not covered by health insurance, and services covered are provided in an extremely fair, equal, and inexpensive manner. Free-access is guaranteed, and Japan was the first in the world to establish a systematic long-term care insurance system (3).
日本的医疗保健体系在国际上享有盛誉,该国在 20 世纪 60 年代就实现了全民医保。几乎没有什么治疗不在医疗保险覆盖范围内,而且所提供的服务极其公平、平等且价格低廉。日本保证免费就医,并且是世界上第一个建立系统性长期护理保险制度的国家( 3 )。
The World Health Organization report in 2000 (4), a Newsweek feature in 2010 (5), and The Lancet in 2011 (6), international media and organizations speak highly of Japan's healthcare delivery system. On the other hand, however, the Lancet points out, for example, that Japan is facing a declining birthrate and an aging population, and there is no guarantee that the current system can be maintained in such an environment. This is a very good system, but if it is to be maintained, it must be reformed.
世界卫生组织 2000 年的报告( 4 )、《新闻周刊》2010 年的专题报道( 5 )以及《柳叶刀》2011 年的专题报道( 6 ),国际媒体和组织都高度评价了日本的医疗保健体系。然而,另一方面,《柳叶刀》指出,例如,日本正面临少子老龄化问题,现有体系在这样的环境下能否维持下去,并无定论。这是一个很好的体系,但如果要维持下去,就必须进行改革。
Issues surrounding Japan's medical care: Challenges of a "super-aged" society
日本医疗问题:“超高龄社会”的挑战
Japan is already one of the world's most aged societies, its population declining by 800,000 to 1,000,000 people every year (7). There are no signs of any reversal to this decline, or to the aging of the population. Japan's population is expected to decline by about 15% by 2040 (7). On the other hand, the number of elderly people, especially those in the later stages of life, will increase, so the growth in the number of people requiring nursing care will outpace that of the overall aging of the population. Japan's elderly population will peak in 2040, and its super-elderly population in the 2060s (8), so numbers of individuals requiring care will not start to ease until after that time.
日本已是世界上老龄化程度最高的社会之一,其人口每年减少 80 万至 100 万人 ( 7 )。目前尚无迹象表明这种下降趋势或人口老龄化趋势会有所逆转。预计到 2040 年,日本人口将减少约 15% ( 7 )。另一方面,老年人口(尤其是老年老年人口)的数量将会增加,因此需要护理的人数增长速度将超过人口整体老龄化的速度。日本老年人口将在 2040 年达到顶峰,超老年人口将在 2060 年代达到顶峰 ( 8 ),因此需要护理的人数要到那之后才会开始减少。
In addition, the structure of diseases will change. The number of chronic diseases will increase, pushing up treatment rates and length of treatment. The length of time people require nursing care will also increase. In other words, medical care needs per capita will increase.
此外,疾病结构将发生变化。慢性病数量将增加,从而推高治疗率和治疗时长。人们需要护理的时间也将增加。换句话说,人均医疗保健需求将会增加。
Furthermore, medical technology is advancing at an ever-increasing pace, so medical care will become more sophisticated, and diseases that could not be cured before will be cured. If diseases can be cured, the average life expectancy will further increase.
而且,医疗技术日新月异,医疗水平也会越来越高,以前无法治愈的疾病也能够治愈。如果疾病能够治愈,人类的平均寿命就会进一步延长。
An increase in medical care needs is unavoidable. Recently, Japan's fiscal authorities have argued without evidence that an increase in costs can be kept in line with gross domestic product (GDP) growth, but a look at other countries reveals that this is impossible. The Organization for Economic Co-operation and Development has published research showing that the ratio of medical care costs to GDP will increase over the next 20 years in all developed countries (8). This does not mean that nothing can be done about costs, but as long as there is a substantive increase in needs, an increase in medical care costs should be considered inevitable.
医疗需求的增长不可避免。最近,日本财政当局毫无根据地声称,医疗成本的增长可以与国内生产总值 (GDP) 的增长保持一致,但看看其他国家的情况就知道,这是不可能的。经济合作与发展组织 (OECD) 发布的一项研究表明,未来 20 年,所有发达国家的医疗成本占 GDP 的比率都将上升 ( 8 )。这并不意味着对成本无能为力,但只要需求大幅增长,医疗成本的上涨就不可避免。
Meanwhile, the socioeconomic structure of Japan and the profile of its elderly population continue to evolve. Family and community ties are weakening, and the number of elderly living alone or in pairs will increase. Already today, most of Japan's elderly are already in single- or two-person households. This means that the point at which support is necessary is getting closer and closer to individuals. For example, a helper must be dispatched if an elderly person living alone needs something as small as a lightbulb changed. The proportion of the elderly who depend on public services will continue to increase.
与此同时,日本的社会经济结构和老年人口结构正在不断演变。家庭和社区纽带正在减弱,独居或双人居住的老年人数量将会增加。如今,日本大多数老年人已经生活在单人或双人家庭中。这意味着需要帮助的阶段越来越接近个人。例如,即使是独居老人需要更换灯泡之类的小事,也必须派遣一名帮手。依赖公共服务的老年人比例将继续增加。
Since the postwar generation will become the core of Japan's elderly population, a majority will be made up by long-time urban residents and Employees' pensioners. On the other hand, however, income disparities within the elderly population will widen.
由于战后一代将成为日本老年人口的主体,其中大部分将由长期居住在城市的人和退休人员构成。然而,另一方面,老年人口内部的收入差距将会扩大。
In addition, the post-bubble generation, who were of working age during Japan's 30 years of economic stagnation, and those over 40 who struggled to find work and became contract employees, will grow old. The number of elderly people who are single, poor, and without relatives will increase. The burden on the social security system will continue to grow.
此外,泡沫破灭后的一代人,也就是在日本经济停滞的30年里处于劳动年龄的一代人,以及那些40多岁、努力就业、成为合同工的人,都将步入老龄化。单身、贫困、无亲无故的老年人口数量将会增加。社会保障体系的负担将持续加重。
Issues surrounding Japan's medical care: Challenges of human and material resources
日本医疗面临的课题:人力、物力的课题
The level of human and material resources supporting medical care in Japan is surprisingly not very high. If we reiterate the characteristics of Japan's medical care delivery system, the reasons for this become clear.
日本医疗的人力和物力支持水平令人惊讶地不高。如果我们重温一下日本医疗体系的特点,就会明白其中的原因。
i) Japan has the most private capital-dependent healthcare delivery system of any developed country. Profits and losses of private hospitals ultimately belong to individuals (medical corporations) who manage those corporations at their own risk. Furthermore, even if the hospital is a non-profit corporation, the president of the hospital must act as a personal guarantor for any capital investment, no different from any other small business. Because they are managed by individuals who guarantee their debts, they cannot be easily reorganized and integrated.
i ) 日本是发达国家中医疗体系对私人资本依赖程度最高的国家。 私立医院的盈亏最终归属于个人(医疗机构),他们自行承担风险管理这些机构。此外,即使医院是非营利性机构,院长也必须为所有资本投资提供个人担保,这与其他小型企业并无二致。由于这些机构由个人管理,并由个人为其债务提供担保,因此很难进行重组和整合。
ii) Governance of the regional healthcare provision system is not yet established. Until the revision of the Medical Service Act in 1985, it was not even possible to regulate the number of hospital beds. The allocation of human and material resources and capital investment is done by individual medical institutions based on their own judgment. In other words, they are facility-complete, and not "community-complete", in which the entire region coordinates and maintains its own facilities.
ii ) 区域医疗服务体系的治理机制尚未建立。 直到 1985 年《医疗服务法》修订之前,甚至连病床数量都无法监管。人力、物力和资本投资的分配都由各个医疗机构自行决定。换句话说,它们是设施齐全型的,而不是由整个区域协调和维护自身设施的“社区齐全型”。
Not only private hospitals, but also public hospitals and public medical institutions, which are supposed to be well governed, duplicate functions and investments, wasting resources. In addition, medical institutions have undifferentiated functions and don't sufficiently coordinate between each other. As a result, although the number of hospital beds in Japan is high by international standards, higher functions are weak, medical care functions are inadequate, and there is no coordination with long-term care.
不仅私立医院,就连理应管理完善的公立医院和公立医疗机构也存在职能和投资重复的问题,造成资源浪费。此外,医疗机构职能划分不清,彼此之间协调不足。因此,尽管日本的病床数量在国际上处于领先地位,但高级职能薄弱,医疗职能不足,并且与长期护理部门缺乏协调。
The number of doctors per population in Japan is not so bad, but the number of doctors per hospital bed is only one-fifth of those in the U.S. and the U.K., and less than half of those in Germany and France (Figure 1 and Figure 2). In addition, the number of doctors per hospital bed in other countries is increasing significantly as medical care becomes more sophisticated. The number of doctors per hospital bed in Japan has hardly increased at all, the gap between Japan and other countries is growing wider and wider; and the same is true for nursing staff (Figure 2).
日本的人均医生数量还算可以,但每张病床的医生数量仅为美国和英国的五分之一,不到德国和法国的一半( Figure 1 和 Figure 2 )。此外,随着医疗保健的日益完善,其他国家每张病床的医生数量也在显著增加。而日本每张病床的医生数量几乎没有增加,日本与其他国家之间的差距越来越大;护理人员的数量也是如此( Figure 2 )。
Figure 1. 图 1.
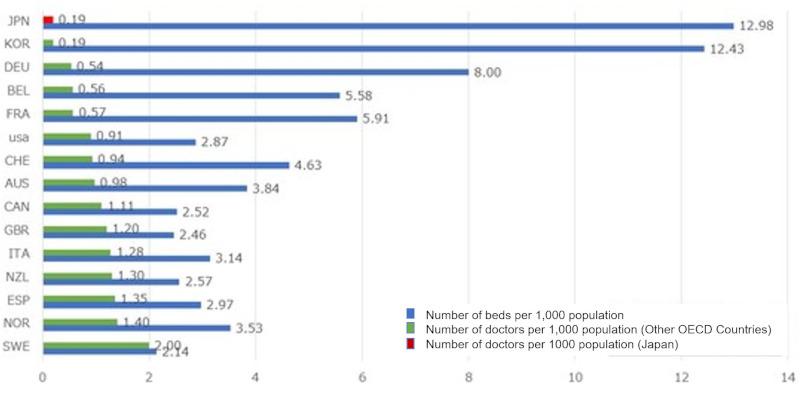
The number of physicians per hospital bed in Japan.
Data Source: OECD Health Statistics 2018. https://www.oecd-ilibrary.org/social-issues-migration-health/data/oecd-health-statistics_health-data-en
日本每张病床的医生数量。 数据来源:经合组织卫生统计数据 2018。https://www.oecd-ilibrary.org/social-issues-migration-health/data/oecd-health-statistics_health-data-en
Figure 2. 图 2.
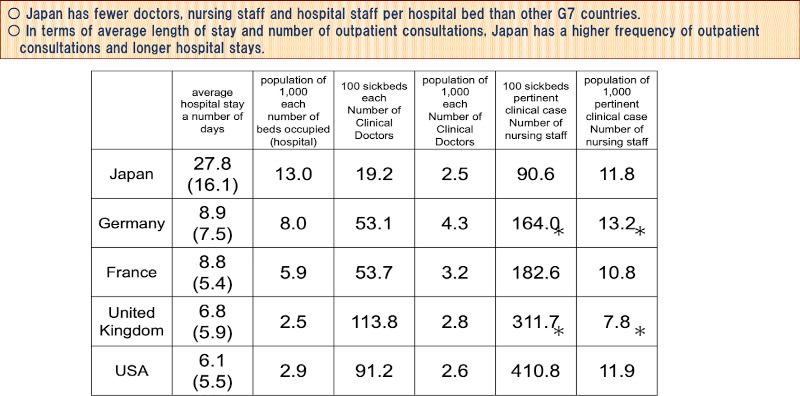
International comparison of the Number of hospital staff per hospital bed, average length of stay and discharge in G7 countries. *includes staff working at research institutes, etc., in addition to staff actually engaged in clinical practice. Data Source: Ministry of Health, Labour and Welfare. Survey of medical facilities (2020). https://www.mhlw.go.jp/bunya/iryouhoken/ database/zenpan/iryoukikan.html
七国集团(G7)每张病床的医护人员数量、平均住院日数及出院日数的国际比较。 *除实际从事临床实践的人员外,还包括在研究机构等机构工作的人员。 数据来源:厚生劳动省。医疗机构调查(2020 年)。https://www.mhlw.go.jp/bunya/iryouhoken/database/zenpan/iryoukikan.html
This is reflected in the difference in the average length of hospital stay. Although the hospital stay in Japan has become much shorter, it is still longer than in the West. It is well known that the length of hospital stay is correlated, or rather inversely related, to the number of doctors in a hospital. In short, in Japan, hospital care has become "thin-on-the-ground medical care".
这反映在平均住院时间的差异上。虽然日本的住院时间已经大幅缩短,但仍然比西方国家长。众所周知,住院时间与医院的医生数量呈正相关,或者更确切地说是反比。简而言之,在日本,医院护理已成为“单薄的医疗”。
Looking at the percentage of hospitals by type of establishment (Figure 3), 93% of private hospitals have 199 beds or less (9). These hospitals account for 70% of Japan's total (9). The fact that there are many medical facilities and patients can go where they choose, and that there are medical facilities close by, means that it is easy to get medical care, but the question remains as to whether this is the case from the perspective of allocating finite medical resources.
从各类型医院的占比来看( Figure 3 ),93%的私立医院床位数量不超过 199 张( 9 )。这类医院占日本全国医院总数的 70%( 9 )。医疗机构众多,患者可以自行选择就诊地点,而且附近也有医疗机构,这意味着就医十分便捷。但从分配有限医疗资源的角度来看,情况是否如此,仍是一个疑问。
Figure 3. 图 3.
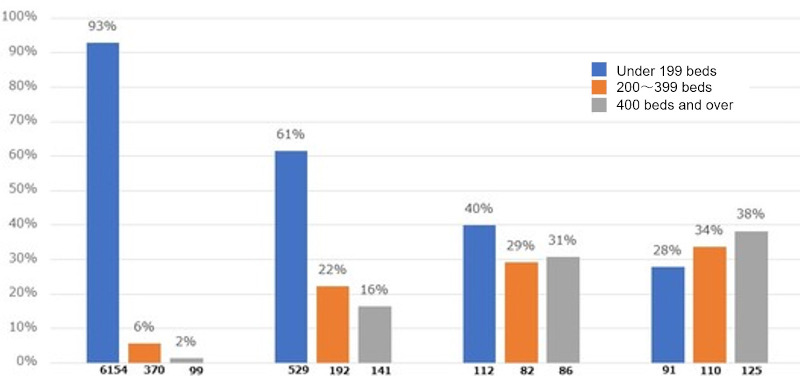
Percentage of hospitals by type of establishment and bed size. Hospitals in Japan are small in size. In particular, more than 90% of private hospitals have less than 200 beds. Data Source: Ministry of Health, Labour and Welfare. Survey of medical facilities (2020). https://www.mhlw.go.jp/bunya/iryouhoken/database/zenpan/iryoukikan.html
按机构类型和床位规模划分的医院百分比。 日本的医院规模较小。尤其是超过 90%的私立医院床位不足 200 张。 数据来源:厚生劳动省。《医疗机构调查》(2020 年)。https://www.mhlw.go.jp/bunya/iryouhoken/database/zenpan/iryoukikan.html
A simple calculation shows that each hospital physician is responsible for 5.5 inpatients in Japan, in other words, one doctor is in charge of 5.5 beds. In the U.S., the number is 1.1. This means that Japanese hospital physicians are responsible for five times as many patients as their American counterparts.
简单计算一下,日本医院每位医生负责5.5名住院病人,也就是5.5张床位。而美国是1.1张。这意味着日本医院医生负责的病人数量是美国医生的5倍。
In the outpatient setting, the total number of outpatient visits per year by U.S. physicians is 1,538, compared to 5,333 in Japan (10). Under the Japanese healthcare system, which guarantees free access, the working environment for doctors is extremely harsh. It would be strange if reforming physicians' working environment was not on the table.
在门诊方面,美国医生每年门诊总人次为 1,538 人次,而日本( 10 )仅为 5,333 人次。在保障免费医疗的日本医疗体系下,医生的工作环境极其恶劣。如果医生的工作环境没有改革的可能,那才叫奇怪呢。
Why is this happening? Since the achievement of universal health insurance, Japan has not developed enough human and material resources to meet exploding medical needs. The history of medical care demand has been handled mainly by private medical institutions with minimal facilities and manpower. Looked at from a different perspective, the system of fee-for-service payment, may also be said to solve the problem by simply encouraging the creation of more medical institutions.
为什么会出现这种情况?自全民医保实现以来,日本一直未能投入足够的人力和物力来满足激增的医疗需求。历史上,医疗需求主要由设施和人力匮乏的私立医疗机构承担。换个角度来看,按服务付费制度或许也可以说只是通过鼓励更多医疗机构的设立来解决问题。
Hospital doctors and staff are chronically overworked, but unable to provide concentrated inpatient care; diagnosis responsibilities are undifferentiated and hospitals are unable to keep up with changes in the kinds of diseases that patients present. Many medical institutions don't have the facilities or the staff to provide advanced functions.
医院的医生和工作人员长期处于超负荷状态,却无法提供集中的住院治疗;诊断职责不明确,医院无法跟上患者病情的变化。许多医疗机构缺乏提供先进功能的设施和人员。
Nevertheless, since the medical care delivery system is built on the premise that medical institutions are self-financed, the entire system will collapse if reimbursement is not designed so that each medical institution can operate independently. As a consequence, various policy inducements have been made, but the remuneration system (allocation of financial resources) has largely been set up to maintain the status quo.
然而,由于医疗体系建立在医疗机构自负盈亏的前提下,如果不设计让各医疗机构能够独立运作的报销机制,整个体系就会崩溃。因此,尽管出台了各种政策激励措施,但薪酬制度(财政资源分配)的设定基本上是为了维持现状。
The problems inherent in this structure were exposed in one fell swoop with COVID-19.
这种结构固有的问题在新冠疫情中一下子暴露无遗。
What we learned in the COVID-19 pandemic
我们从新冠疫情中学到的东西
Although there are various opinions, mine is that what Japan experienced during the COVID-19 pandemic gives a glimpse of what Japan's medical care will look like 20 years from now.
尽管存在各种各样的观点,但我认为,日本在新冠疫情期间的经历可以让我们一窥20年后日本的医疗保健状况。
Even today, 70% of hospitalized patients are already over 65 years old. Half of them are over 75 years old (11). In 20 years, most patients will require nursing care and have underlying diseases. A large percentage of them will have dementia. It will be the norm for such people to come in with infections, acute exacerbations, pneumonia, and broken bones - and there is no one at home to take care of them.
即使在今天,70% 的住院患者也已经超过 65 岁。其中一半超过 75 岁( 11 )。20 年后,大多数患者将需要护理,并且患有基础疾病。其中很大一部分患者将患有痴呆症。这些人因感染、急性加重、肺炎和骨折入院将成为常态——而且家中无人照顾他们。
We have to think about the medical and nursing care system with such patients in mind. The plan was to get there by 2040, but this situation is now unfolding before our eyes. Remember what happened in the infectious disease ward when an elderly dementia patient was hospitalized with the coronavirus? In 2040, such situations ― while the majority of patients admitted to acute care hospitals are those in need of care with multiple underlying medical conditions at the same time ― will occur on a large scale on a daily basis.
我们必须将这类患者纳入医疗和护理体系的考量。我们原本计划在2040年实现这一目标,但现在这种情况正在我们眼前上演。还记得传染病房里一位老年痴呆症患者因感染新冠病毒住院时发生的情况吗?虽然大多数急症护理医院收治的患者都同时患有多种基础疾病,但到了2040年,这种情况将大规模地、每天都在发生——尽管大多数急症护理医院收治的患者都同时患有多种基础疾病。
If this is the case, medical and nursing capabilities must be thought of together. A unilinear regional care delivery system with hospitals at its core, with the hospital upstream and the home care system downstream, will no longer be possible. Acute care hospitals must also consider having medical and long-term care capabilities, and chronic care hospitals must be able to provide at least secondary emergency care in order to support the community.
如果真是这样,医疗和护理能力必须一并考虑。以医院为核心,医院上游、家庭护理系统下游的单线区域医疗服务体系将不再可行。急症护理医院也必须考虑具备医疗和长期护理能力,慢性病护理医院必须至少具备二级紧急护理能力,才能为社区提供支持。
Nursing homes, as well, cannot skimp on medical care capabilities. The entire home care provision system will literally break down if a comprehensive and coherent care network is not implemented.
养老院同样不能吝惜医疗资源。如果无法构建一个全面、连贯的护理网络,整个居家养老服务体系将彻底崩溃。
These things have been discussed for a long time, but unless they are seriously implemented now, we will not be able to survive in the future society. The pandemic forced this realization upon Japan by exposing structural problems in its healthcare delivery system.
这些事情已经讨论了很久,但如果现在不认真落实,我们将无法在未来的社会中生存。疫情暴露了日本医疗体系的结构性问题,迫使人们认识到了这一点。
Of course, a pandemic is a one-off, large-scale disaster that does not happen every day. In that sense, it is correct to consider Japan's "contingency response". At the same time, the situation that occurred - the so-called "collapse of medical care" - should be viewed as the manifestation of structural problems that were inherent in the system during normal times, and as an opportunity to solve structural problems in the current healthcare delivery system itself.
当然,疫情大流行是一次性的大规模灾难,并非每天都会发生。从这个意义上讲,日本的“应急应对”是正确的。同时,所谓的“医疗崩溃”应该被视为正常时期医疗体系固有结构性问题的体现,同时也是解决现有医疗体系自身结构性问题的契机。
The reasons that Japan's system of delivering medical care is functionally undifferentiated, inefficient, "thinly spread", and lacking in spare capacity is precisely because medical care has been delivered mainly by independently-financed private hospitals in an unrestricted medical system where doctors can freely select their own medical specialties and disclose them to the public (free labeling). Cooperation and collaboration among medical institutions is not the default, and any cooperation among doctors and medical institutions is basically left to the resourcefulness and actions of individual doctors and medical institutions on the frontline.
日本医疗体系之所以功能单一、效率低下、“分散”且缺乏剩余能力,正是因为医疗服务主要由自费的私立医院提供,在不受限制的医疗体系下,医生可以自由选择自己的专业并向公众公开(自由标签)。医疗机构之间的合作与协作并非默认,医生和医疗机构之间的任何合作,基本上都取决于一线医生和医疗机构的智慧和行动。
Furthermore, under a free-access medical insurance system with a high degree of freedom of choice on the part of patients, there is no institutional control of patient flow. In Japan's free access system, patients are entirely responsible for deciding whether or not to go to a doctor, which doctor to go to, and which department to go to, without any advice or assistance from professional medical personnel. In other words, the system is not designed to objectively provide timely and appropriate medical care or to provide necessary medical care when needed. If this is the case, it is difficult to create a system for comprehensive and continuous health management, a flow of prevention and health management, initial diagnosis and treatment (primary care), specialized treatment, return home, and nursing care and lifestyle support. In other words, neither the supply, nor the demand side can be controlled.
此外,在患者选择自由度较高的自由就医制度下,患者流动缺乏制度上的控制。在日本的自由就医制度下,患者完全由自己决定是否就医、去哪位医生、去哪个科室就医,没有任何专业医务人员的建议或帮助。换言之,该制度的设计并非客观地提供及时且合适的医疗服务,或在需要时提供必要的医疗服务。如果如此,就难以构建一个全面且持续的健康管理体系,难以形成预防和健康管理、初期诊疗(初级保健)、专科治疗、回家、护理和生活支持的流程。换言之,无论是供给侧还是需求侧都无法控制。
Despite this situation, the system has managed to function to date. However, the frontline healthcare workers who support medical care shoulder a heavy burden. As mentioned above, the number of inpatients per physician in Japan is five times that of the U.S., and the total number of outpatients per year is 3.5 times that of the U.S. As the recent pandemic has made clear, Japan's healthcare system is fragile and can easily collapse if there is two much pressure put on one specific point.
尽管如此,该系统迄今为止仍勉强维持运转。然而,支撑医疗的一线医护人员却肩负着沉重的负担。如上所述,日本每位医生的住院病人数量是美国的5倍,每年门诊病人总数是美国的3.5倍。正如最近的疫情所表明的那样,日本的医疗体系非常脆弱,如果对某一点施加过大的压力,就很容易崩溃。
Will medicine really be able to sustain itself for the next 15 to 20 years in Japan? Even now, there are cases of emergency patients being shunted around from hospital to hospital and individuals who are unable to access medical care and nursing care. The lack of coordination and networking on the provider side has led to blockages here and there, and there have been many cases of families running around looking for a facility to stay in.
在日本,医疗真的能够在未来15到20年持续下去吗?即使是现在,急诊病人也经常被辗转于不同的医院,无法获得医疗和护理。医疗机构方面缺乏协调和网络,导致各种问题频发,许多家庭不得不四处寻找合适的住所。
Now that the pandemic has brought the problem to the fore, perhaps now is the time for reform.
如今,疫情使这个问题凸显出来,或许现在正是改革的时候。
What is required of medical care in a super-aged society
超高龄社会对医疗有何要求
In the long-term care world, it's already common understanding that the goal of elderly care should be to enable people to live with dignity at home, in their community, for as long as possible (12). The role of long-term care service is to support lives and lifestyles. In a super-aged society, regular medical practitioners need to also start thinking this way.
在长期护理领域,养老服务的目标应该是让人们尽可能长时间地在家中、在社区中享受有尊严的生活,这已是共识 ( 12 )。长期护理服务的作用在于支持生活和生活方式。在超高龄社会,普通医护人员也需要开始这样思考。
The basic function of medicine - providing treatment to cure - will not change, but in addition to that, it will be important to heal and support. In other words, what will be required is medical care that supports the dignity of people's lives, and does not sacrifice life for the sake of treatment. Medical care will exist as a part of life.
医疗的基本功能——通过治疗治愈——不会改变,但除此之外,治愈和支持也变得至关重要。换句话说,我们需要的是维护生命尊严的医疗,而不是为了治疗而牺牲生命。医疗将作为生命的一部分而存在。
"Healing and support" cannot be achieved by medical care alone, unless a comprehensive regional care network, provided by medical care and long-term care together, with the cooperation of many different professions that support patients, is created.
“治愈和支持”不能仅靠医疗手段实现,必须建立由医疗和长期护理共同提供的、由众多支持患者的不同专业合作的综合区域护理网络。
As is already the case in the world of social service and, outreach to patients/users in close proximity will also be required of medical care. House calls will become more important, and asynchronous, remote medical care, such as telemedicine, will become an important weapon in the future, especially when considering the limited human and material resources available to support local medical care. There have been remarkable advances in medical digital transformation and other home healthcare support technologies, and it is already technically possible to perform a considerable amount of diagnostic procedures remotely (13). These technological innovations will contribute to reducing the burden on both patients and medical personnel, and should be actively implemented.
正如社会服务领域已经出现的情况一样,医疗保健领域也需要近距离接触患者/用户。上门服务将变得更加重要,而异步远程医疗(例如远程医疗)将成为未来的重要武器,尤其是在考虑到支持本地医疗的人力和物力资源有限的情况下。医疗数字化转型和其他家庭医疗保健支持技术已经取得了显著进展,并且在技术上已经可以远程执行大量诊断程序( 13 )。这些技术创新将有助于减轻患者和医务人员的负担,应该积极实施。
In order for this system to work, IT infrastructure to centralize patient health information and share information, is an indispensable prerequisite. "Tooling" such as medical IT, IoT, and digital transformation must be standard, and should be prioritized as essential to support home medical care and community comprehensive and coherent care networks.
为了使该系统发挥作用,用于集中管理患者健康信息并共享信息的 IT 基础设施是必不可少的前提条件。医疗 IT、物联网和数字化转型等“工具”必须标准化,并应优先考虑,以支持居家医疗和社区综合连贯的护理网络。
Medical care challenges faced by a super-aged society
超高龄社会面临的医疗挑战
The functions of hospitals in a super-aged society will be divided into two major approaches. On one hand will be highly-specialized, acute care hospitals that provide intensive acute care, on the other, community-based hospitals that provide medical care for healing and support (3).
超高龄社会中的医院职能将大致分为两大类。一类是提供重症急性护理的高度专业化的急性护理医院,另一类是提供康复和支持医疗服务的社区医院( 3 )。
While there has been a lot of discussion about rethinking regional medical care, we should further promote functional differentiation of hospital beds, selection and concentration, strengthening of acute care functions, and concentrated investment of resources (efficient use of hospital beds by reducing the number of hospital beds). At the same time, we should also clearly set a direction for strengthening regional medical care and home medical care. As I have emphasized in this paper, if home medical care is not strengthened, the burden on hospitals and emergency medical services will increase, and the entire medical care delivery system will break down.
虽然关于重新思考区域医疗的讨论很多,但我们应该进一步推进病床功能分化、精选和集中、强化急诊功能以及资源集中投入(通过减少病床数量来高效利用病床)。同时,我们也应该明确加强区域医疗和居家医疗的方向。正如我在本文中强调的那样,如果不加强居家医疗,医院和急救医疗的负担就会加重,整个医疗服务体系就会崩溃。
In this sense, the implementation of primary care physician function and the clarification of the functions and roles of small and medium-sized community-based hospitals that support this function, as well as the establishment of a regional comprehensive and coherent care network with multidisciplinary cooperation that transcends medical care, should also be pillars of regional medical care.
从这个意义上来说,落实初级保健医生职能、明确支持该职能的中小型社区医院的功能和作用,以及建立超越医疗范畴、多学科合作的区域综合连贯的医疗网络,也应当成为区域医疗的支柱。
Regional medical care impacts the overall medical care delivery system. Although debate tends to focus on reducing the number of hospital beds, the original purpose of regional medical care is to reallocate and reorganize human and physical resources to "efficiently meet the future medical (and nursing care) needs of the region with the existing human and physical resources".
区域医疗影响着整个医疗体系。尽管争论的焦点往往集中在减少病床数量上,但区域医疗的初衷是重新配置和重组人力和物力资源,以“利用现有的人力和物力资源,高效地满足该地区未来的医疗(和护理)需求”。
The realization of better regional medical care will lead to better resource allocation and the optimization of overall medical care costs. Reforming how care is delivered is the most realistic and effective way to optimize costs.
实现区域医疗优生,有利于资源配置的优化,也有利于医疗成本的优化。改革医疗服务方式,是优化成本最现实、最有效的途径。
Long-term care becomes more important in a super-aging society
超级老龄化社会中长期护理变得更加重要
Finally, I would like to share some interesting data. As you may recall, all elderly people aged 65 and over are enrolled in Medicare in the US. In other words, all medical costs for the US population after the age of 65 are reflected in the Medicare database.
最后,我想分享一些有意思的数据。大家可能还记得,美国所有 65 岁及以上的老年人都参加了 Medicare。也就是说,美国 65 岁以后所有人口的医疗费用都反映在 Medicare 数据库中。
One study (14) compares the cumulative amount of medical and long-term care expenses spent by those aged 65 or older who are enrolled in Medicare up to the time of their death, segmented by age at death. The data shows that the longer a person lives, the more his/her lifetime medical expenses increase until they peak out at around age 90-95. In other words, the lifetime medical costs of someone who lives to be 100 or and someone who lives to be 110 years old are not very different. It follows, then, that if average life expectancy were to increase to 90 or 100 years, medical costs would gradually start to peak out as people lived longer healthy lives.
一项研究 ( 14 ) 比较了 65 岁或以上参加 Medicare 的老年人在其去世前累计的医疗和长期护理费用,并按死亡年龄进行细分。数据显示,人的寿命越长,其终生医疗费用就越高,直到 90-95 岁左右达到峰值。换句话说,活到 100 岁和活到 110 岁的人的终生医疗费用差别并不大。因此,如果平均预期寿命增加到 90 岁或 100 岁,随着人们健康生活的延长,医疗费用将逐渐开始达到峰值。
The data for long-term care costs shows a different picture. The lifetime cost of long-term care increases with the age at death, and exceeds the lifetime cost of medical care for those over age 95. This means that as more people age in a super-aged society, the relationship between cumulative medical costs and cumulative long-term care costs by the time of death is reversed.
长期护理费用的数据则呈现出不同的景象。长期护理的终生成本随着死亡年龄的增长而增加,对于95岁以上的人来说,其终生成本甚至超过了医疗保健。这意味着,随着超高龄社会中人口老龄化,累计医疗费用和累计长期护理费用之间的关系会发生逆转。
In other words, aging (increase in life expectancy) will be a factor in increasing lifetime medical costs until about the age of the 90s, but long-term care (long-term care) will continue to grow without peaking out.
也就是说,老龄化(寿命延长)在90岁左右之前都会成为一生医疗费用增加的一个因素,但长期护理(长期护理)将持续增长而不会达到峰值。
In conclusion, The COVID-19 disaster revealed structural weaknesses in Japan's healthcare delivery system. We should take this as an important warning: this is only the beginning. Looking ahead to the year 2040, it is inevitable that Japan will need to streamline and optimize its healthcare delivery system given its limited resources. This will depend on a reform of the entire regional medical care delivery system, and a move towards a more community approach to medical care. Only this shift will allow Japan to more efficiently use resources and give patients better care - and a shot at a better quality of life - overall.
总而言之,新冠疫情暴露了日本医疗体系的结构性缺陷。我们应该将此视为一个重要的警示:这仅仅是个开始。展望2040年,鉴于日本有限的资源,精简和优化其医疗体系势在必行。这将取决于整个区域医疗体系的改革,以及向更加社区化的医疗模式转变。只有这种转变才能使日本更有效地利用资源,为患者提供更好的护理,并最终提高整体生活质量。
Funding 资金
None. 没有任何。
Conflict of Interest 利益冲突
The author has no conflicts of interest to disclose.
作者没有需要披露的利益冲突。
References 参考
-
1.
Cabinet Secretariat (Japan). Report of National Council for Social Security Reform, 2013.
https://www5.cao.go.jp/keizai-shimon/kaigi/minutes/2013/0808/sankou_02.pdf (accessed November 21, 2023). (in Japanese) .
1. 日本内阁官房。《国家社会保障改革委员会报告》,2013 年。 https://www5.cao.go.jp/keizai-shimon/kaigi/minutes/2013/0808/sankou_02.pdf (2023 年 11 月 21 日访问)。(日语)。 -
2.
Shuhei Ikai. A Theory of the Hospital Century.
Yuhikaku Publishing, Tokyo, Japan. 2010. [Google Scholar]
2. 井修平。医院世纪的理论。 Yuhikaku 出版社,日本东京。 2010。 [ Google Scholar ] -
3.
Ministry of Health, Labour and Welfare. White Paper on Health, Labour and Welfare (2000).
https://www.mhlw.go.jp/toukei_hakusho/hakusho/kousei/2000/ (accessed January 16, 2024). (in Japanese) .
3. 厚生劳动省。《厚生劳动福利白皮书》(2000 年)。 https://www.mhlw.go.jp/toukei_hakusho/hakusho/kousei/2000/ (2024 年 1 月 16 日访问)。(日语)。 -
4.
World Health Organization. The world health report 2000. Health Systems: Improving Performance.
https://www.who.int/publications/i/item/924156198X (accessed November 21, 2023).
4. 世界卫生组织。《2000 年世界卫生报告》。卫生系统:提升绩效。 https://www.who.int/publications/i/item/924156198X (2023 年 11 月 21 日访问)。 -
5.
Newsweek. The best countries in the world (August 16, 2010).
https://www.newsweek.com/best-countries-world-71817 (accessed November 21, 2023).
5. 《新闻周刊》。世界上最好的国家(2010 年 8 月 16 日)。 https://www.newsweek.com/best-countries-world-71817 (2023 年 11 月 21 日访问)。 -
6.
The Lancet. Japan: Universal health care at 50 Years.
https://www.thelancet.com/series/japan (accessed November 21, 2023). [DOI] [PubMed]
6. 《柳叶刀》。日本:全民医疗保健五十年。 https://www.thelancet.com/series/japan (2023 年 11 月 21 日访问)。 [ DOI ] [ PubMed ] -
7.
National Institute of Population and Social Security Research. Population projections for Japan: 2021-2070 (2023).
https://www.ipss.go.jp/site-ad/index_english/population-e.html (accessed January 16, 2024).
7. 国立社会保障与人口问题研究所。《日本人口预测:2021-2070》(2023 年)。 https://www.ipss.go.jp/site-ad/index_english/population-e.html (2024 年 1 月 16 日访问)。 -
8.
OECD iLibrary. Health at a grance 2019: OECD indicators.
https://www.oecd-ilibrary.org/sites/4dd50c09-en/index.html?itemId=/content/publication/4dd50c09-en (accessed January 16, 2024).
8. OECD iLibrary。2019 年健康概览:OECD 指标。 https://www.oecd-ilibrary.org/sites/4dd50c09-en/index.html?itemId=/content/publication/4dd50c09-en (2024 年 1 月 16 日访问)。 -
9.
Ministry of Health, Labour and Welfare. Medical facilities survey (2020).
https://www.mhlw.go.jp/toukei/saikin/hw/iryosd/20/dl/09gaikyo02.pdf (accessed January 16, 2024). (in Japanese) .
9. 厚生劳动省。医疗设施调查(2020 年)。 https://www.mhlw.go.jp/toukei/saikin/hw/iryosd/20/dl/09gaikyo02.pdf (2024 年 1 月 16 日访问)。(日语)。 -
10.
OECD iLibrary. OECD health working Paper 2020.
https://www.oecd-ilibrary.org/social-issues-migration-health/oecd-health-working-papers_18152015
10. OECD iLibrary。OECD 卫生工作报告 2020。 https://www.oecd-ilibrary.org/social-issues-migration-health/oecd-health-working-papers_18152015 -
11.
Ministry of Health, Labour and Welfare. Patient survey (2020).
https://www.mhlw.go.jp/toukei/saikin/hw/kanja/20/index.html (accessed January 16, 2024). (in Japanese) .
11. 厚生劳动省。患者调查(2020 年)。 https://www.mhlw.go.jp/toukei/saikin/hw/kanja/20/index.html (2024 年 1 月 16 日访问)。(日语)。 -
12.
Ministry of Health, Labour and Welfare. Elderly care in 2015.
https://www.mhlw.go.jp/topics/kaigo/kentou/15kourei/3.html (accessed January 16, 2024). (in Japanese) .
12. 厚生劳动省。2015 年老年人护理情况。 https://www.mhlw.go.jp/topics/kaigo/kentou/15kourei/3.html (2024 年 1 月 16 日访问)。(日语)。 -
13.
Takao H. Digital Medicine - Current ability and future.
Nikkei BP, Tokyo, Japan, 2022. (in Japanese). [Google Scholar]
13. Takao H. 数字医学——现状与未来。日经 BP 社,日本东京,2022 年。(日语)。 [ Google Scholar ] -
14.
Spillman BC, Lubitz J. The effect of longevity on spending for acute and long-term care.
N Engl J Med. 2000; 342:1409-1415.
[DOI] [PubMed] [Google Scholar]
14. Spillman BC,Lubitz J. 长寿对急性和长期护理支出的影响。N Engl J Med. 2000;342:1409-1415. [ DOI ] [ PubMed ] [ Google Scholar ]


